Across the U.S., healthcare professionals regularly exchange clinical advice—often informally and without reimbursement. These "curbside consults" are valuable, but unless structured and documented properly, they remain invisible and uncompensated.
That’s changing. Medicare, Medicaid, and commercial insurers now recognize interprofessional consultations—commonly known as eConsults—as billable services. Providers who use secure platforms like Omnidoc can now be paid for their expertise under clear CPT and HCPCS guidelines.
What Is an eConsult?
An eConsult is an asynchronous, provider-to-provider interaction designed to obtain a medical opinion without a face-to-face patient encounter.
It is distinct from:
- Telehealth visits, which require real-time audio-visual contact with the patient,
- Multidisciplinary case conferences, which involve group decision-making,
- Remote patient monitoring, which tracks biometric data over time.
Properly billed eConsults must include a written or verbal request, documented clinical rationale, and either a written or verbal report by the specialist.
CPT Codes for Interprofessional eConsults
CMS recognizes six CPT codes for reimbursable medical eConsults*:
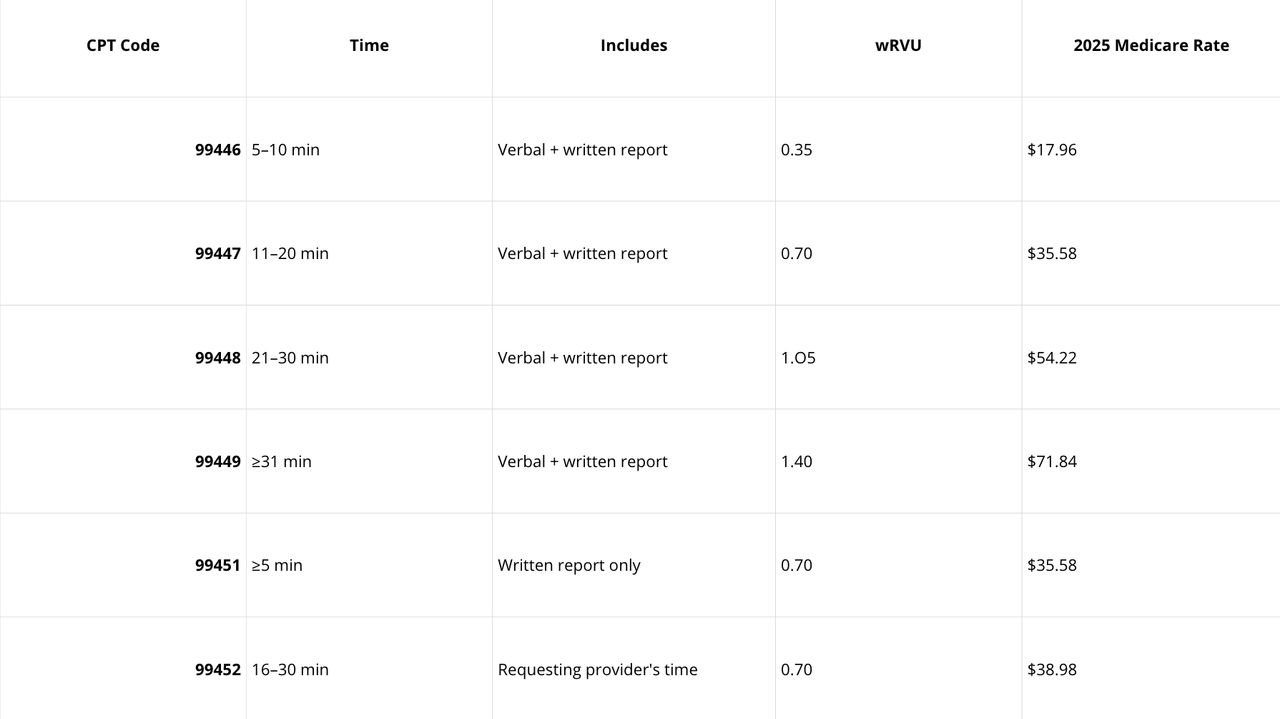
*Reimbursements may vary.
Source: CMS Physician Fee Schedule
HCPCS Codes for Behavioral eConsults (2025)
New in 2025, CMS introduced six behavioral health–specific HCPCS codes to extend eConsult reimbursement* to mental health providers:
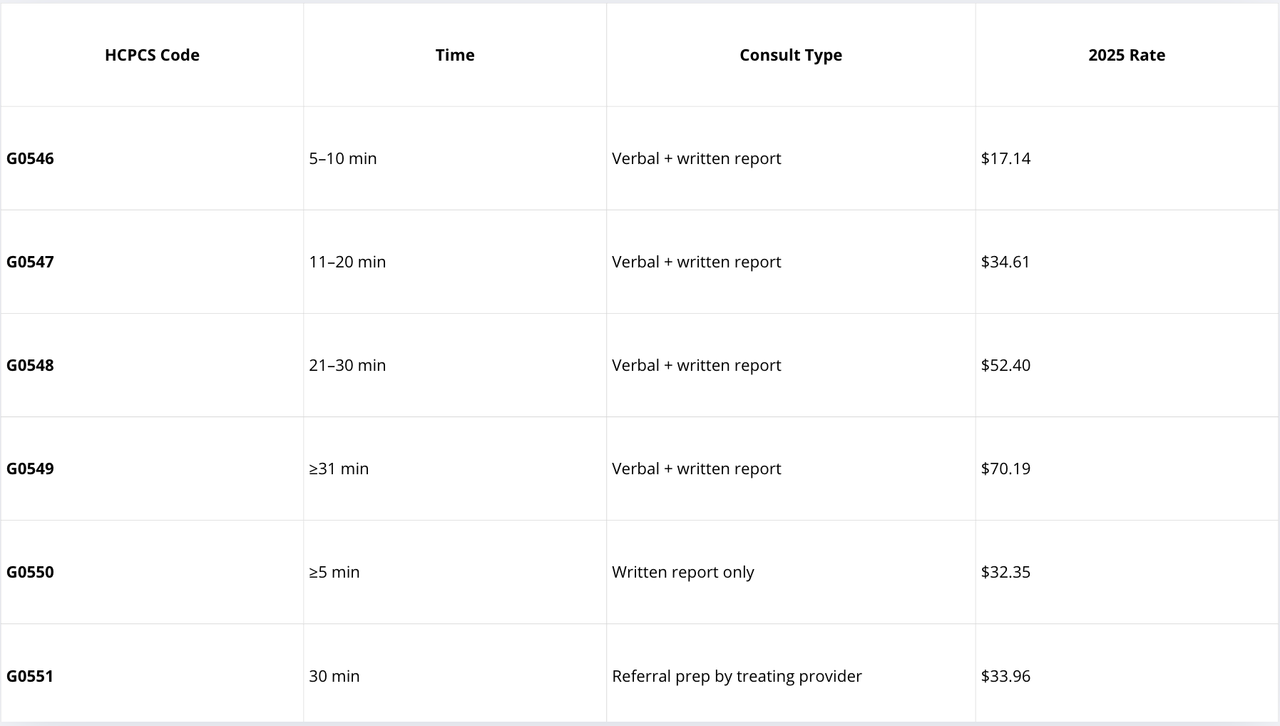
*Reimbursements may vary.
These codes allow participation by behavioral specialists whose services are limited by statute to mental health.
Billing Rules and Documentation Requirements
To be Medicare-compliant, all interprofessional consults must follow these rules:
General Requirements
- Requesting provider must initiate the consult and document the reason.
- Consulting provider must produce a written or verbal report (depending on code).
- Time thresholds must be met as defined by each code.
- Do not report the same code more than once within 7 days (99446–99449) or 14 days (99452) for the same patient.
- Do not bill if the consult results in a face-to-face visit with the consultant within 14 days.
- Patient consent must be obtained and documented by the requesting provider (Medicare requirement).
- Audit-ready documentation includes:
- Date and time of request
- Duration of consultative activities
- Written/verbal report from the consultant
- Confirmation that time was not duplicated with other services
Not allowed: transfer of care, review only (if >50% time spent on chart/data), or use by providers not eligible to bill E/M services (e.g., social workers).
Who Can Bill eConsult Codes?
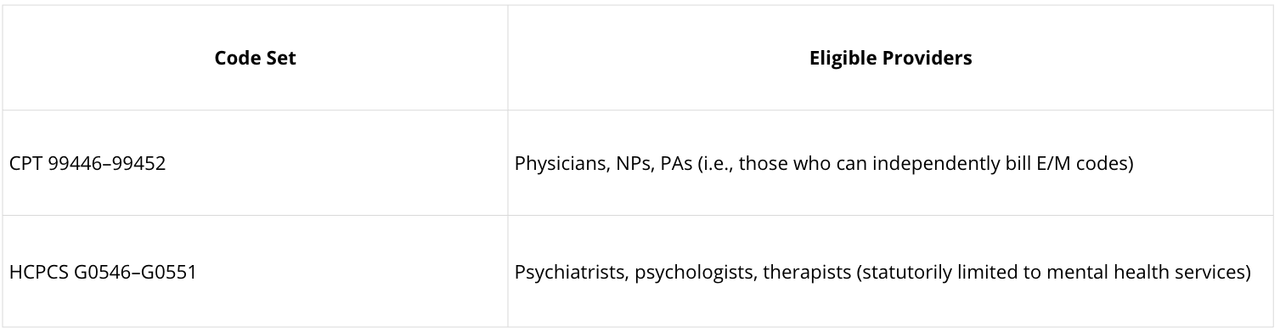
CMS clarified in its 2025 Final Rule that clinical social workers and counselors cannot bill 9945X codes, but may use G-codes under mental health provisions.
How Much Do Private Payers Reimburse?
Reimbursement varies widely across commercial insurers and settings. According to a 2024 study published in the Journal of the Pediatric Infectious Diseases Society:
- Median commercial reimbursement for eConsults: $130.82
- Medicaid median: $40.18
Source: Billing for and Documentation of Provider-to-Provider Interprofessional Consults in Infectious Diseases, Li et al., 2024.
Why Use Omnidoc for eConsults?
Omnidoc guarantees compliance and facilitates billing:
- We ensure regulatory compliance - including HIPAA compliance and audit trails
- We collect all required documentation
- We enable effortless delegation to admin teams - Dedicated interface for staff to manage billing workflows
- We automate through direct connectors - EHR integration through HL7 and FHIR workflows, AI Chart Capture feature, code templates and audit-ready PDF exports.
Ready to Launch a Reimbursable eConsult Program?
Whether you’re part of a hospital system, ACO, or private clinic, Omnidoc helps you structure and scale secure, reimbursable eConsults.
📩 Reach out to us at omnidoc.us to schedule a demo.
For the most up-to-date CPT/HCPCS codes and Medicare payment rates, consult the CMS Physician Fee Schedule. Behavioral health providers can refer to the CMS 2025 Final Rule for full scope of new interprofessional billing options.
